
Medically Reviewed By Dr. Meghav Shah Updated on August 1, 2024
Normal heart rhythm or heart beats occurs regularly between 60 to 100 times per minute. An ECG or electrocardiogram records heart rhythm in the form of electrical impulses. The heart rhythm normally originates in the SA node of the right atria and then these impulses travel through the atria to reach the AV node, situated at the junction of the atria & ventricles and then to the bundle of His, then its left & right bundles and finally into the entire ventricle through the purkinje fibers.
The heart rhythm starts with atrial contraction i.e. a P wave on the ECG followed by ventricular contraction i.e. QRS complex and then finally ventricular relaxation i.e. T waves on the ECG. Any abnormality in this regularity is called an arrhythmia.
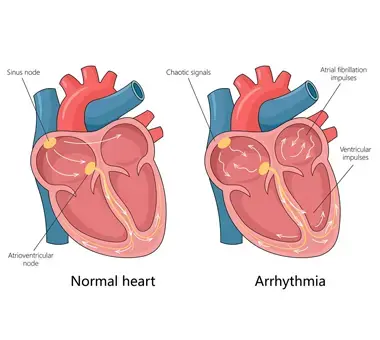
Arrhythmias can be divided broadly into 2 main types based on source of origin. Those origination from the atria (i.e. the upper heart chambers) are called supraventricular arrhythmias. Those originating from the ventricles (i.e. the lower heart chambers) are called ventricular arrhythmias.
These can also be divided broadly into 2 main types based on the heart rate.
Bradyarrhythmias - these types of arrhythmia have heart rates slower than 60 beats per minute.
Tachyarrhythmias - these types of arrhythmia have heart rate higher than 100 beats per minute.
As mentioned previously, these originate from above the ventricles i.e. from any part of the atria or the AV node. In this section we will mainly describe the supra ventricular arrhythmias.
Types of SVA's
Atrial fibrillation
Atrial fibrillation is an irregularly irregular chaotic and usually fast heart rhythm that occurs because of loss of synchronization of the atrial i.e. the upper chamber with the ventricles i.e. the lower chamber of the heart. Usually the atria get enlarged leading to loss or disruption of conduction fibres and thus leading to loss of synchronised atrial activity i.e. absence of P waves on the ECG. This condition, though not directly life threatening, can lead to higher risk of stroke, heart failure and other cardiac conditions.
Atrial flutter
Atrial flutter is a condition where the atrial chamber beats fast and the ECG has a characteristic saw tooth type appearance. This condition is similar to atrial fibrillation in terms of treatment and EP study and ablation for same has better results as compared to atrial fibrillation.
AVNRT and AVRT
Its full forms are AV node re-entrant tachycardia and AV node re-entry tachycardia. In this condition the AV node of the heart or an accessory conduction between the atria and ventricles is responsible for very fast heart rate needing emergency medications in the form of rate reducing injections like adenosine, beta blockers or diltiazem. These conditions need oral beta blockers for a prolonged time and these conditions are too amenable to EP ablation procedures with good long term results.
WPW
It is called Wolff Parkinson White syndrome and is caused by extra conduction fibres connecting the atria to ventricles since birth and is classically associated with short PR segment on the ECG. This condition is also amenable to EP study and ablation.
As mentioned previously, any condition that leads to enlargement of the atria, can cause atrial fibrillation.
Cause are
More often than not, atrial fibrillation is asymptomatic and is diagnosed incidentally when an ECG is done for some other reason or when pulse is felt to be irregular when someone goes to the physician for a check up.
Symptoms can occur in the form of
Paroxysmal - atrial fibrillation occurs intermittently i.e. rhythm is alternating between normal and atrial fibrillation.
Persistent - atrial fibrillation last for more than 7 days.
Long standing/ Permanent - atrial fibrillation last for more than a year and is usually lifelong.
Diagnosis of AFib
ECG is the simplest way to diagnose persistent atrial fibrillation. When paroxysmal, a holter test i.e. an ambulatory heart monitoring may be used to identifying it.
Pharmacology
Heart rate control with betablockers or diltiazem, verapamil or occasionally digoxin. Heart rhythm conversion with anti arrhythmia medicines like amiodarone or flecainide. Blood thinners i.e. anticoagulant medicines like dabigatran, rivaroxaban, edoxaban, apixaban or warfarin.
Surgery
There are some surgical procedures like MAZE or electrophysiology (EP) studies and ablation in form of Pulmonary vein isolation (non open heart surgery) to treat atrial fibrillation.
Electric Cardioversion
This is done by sedating the patient and giving him an external DC cardioversion (shock) to convert atrial fibrillation into sinus rhythm. This is done during emergencies or when pharmacology fails.
Treatment of risk factors like hypertension, diabetes mellitus, weight control. Reduction of caffeine in drinks and stopping use of nicotine. Early diagnosis of atrial fibrillation and prompt treatment with rate control to prevent or reduce symptoms of heart failure.