
Medically Reviewed By Dr. Karan Anandpara Updated on August 1, 2024
Peripheral means affecting your limbs (either upper or lower limbs) and vascular means affecting your circulatory arterial system. Peripheral vascular disease or commonly called PVD, is a circulatory blood vessel disorder affecting the arterial system of your limbs. The arteries may get blocked, narrowed or occluded and the blood flow to your limbs may get compromised. PVD is also called PAD or peripheral arterial disease (PAD).
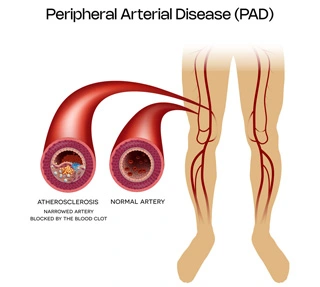
The most common cause is atherosclerosis. Atherosclerosis means the hardening of the arteries and formation of plaques or clots in these vessels. This can be due to old age and high lipid levels/cholesterol levels or due to smoking.
Risk factors for atherosclerosis/PVD include:
Asymptomatic PVD patients may not require any treatment. Blood thinners and a few medications may have to be added to make sure there is no disease progression. This would ideally include Ecosprin and sometimes a low dose anticoagulant like Rivaroxaban may be added.
Claudicants (pain in the legs or arms that occurs while walking or using the arms) may be treated in two ways. For lifestyle non limiting claudicants, conservative management may be tried with blood thinners and exercise programs.
For lifestyle limiting claudication, intervention may be suggested depending on the level of blockage. For short blockages stenting or drug coated balloon angioplasty may be advised. For more complex lesions and blockages, bypass surgery may be suggested. This varies from case to case and treatment is tailored depending on multiple clinical parameters.
Sometimes both surgery and stenting may be combined called “hybrid procedures.” For critical or acute limb ischemia, revascularization to improve the blood flow is essential. This generally involves angioplasty and/or stenting and sometimes combined with a bypass. This requires admission and is followed by a surgical clean up of the wound or ulcer and in extreme cases also require an amputation.
Angioplasty/Stenting for Peripheral Vascular Disease
Reduction of the risk factors for PVD is key
For patients with PVD, you may require to continue your blood thinners life long. It is important for correct foot wear. Wear closed shoes at all time. Socks to be worn at home to prevent wound or hurt to the leg. Prevent extreme hot or cold temperature to the legs to prevent boils and blisters. Any wound to the leg may not heal due to poor blood supply and may end up turning black due to “gangrenous” changes. A dedicated Foot Care regime needs to be followed as a lifestyle modification.