Procedure/Surgery Name: Geniculate Artery embolization for Recurrent Hemarthrosis
Doctors: Dr Bhavesh Arun Popat, Dr Karan M Anandpara
Pre-Op Details & Diagnosis
A 72 years old male
Comorbidities: Morbidly obese, poorly controlled diabetes, hypertensive, previous H/O CABG.
Complaints: Bilateral knee pain, joint aches and soreness (left>right knee).
Pain after joint overuse.
Reduced physical activity and quality of life.
Local knee tenderness +.
X ray bilateral knee s/o bilateral osteoarthritic changes (left more than right).
H/O left sided recurrent hemarthrosis for which percutaneous USG guided aspiration of fluid done outside.
USG local part suggestive of left sided hemarthrosis – hyperechoeic fluid with septations in the left knee joint cavity.
MRI done s/o changes of severe osteoarthritis with left sided hemarthrosis
Pain not relieved by conservative medical management i.e. by anti-inflammatory drugs or corticosteroids.
Not relieved by intra-articular steroid injection.
Not a candidate for joint replacement/arthroplasty in view of significant medical comorbidities, contraindications for general anaesthesia and patient’s refusal for knee arthroplasty.
Treatment Plan
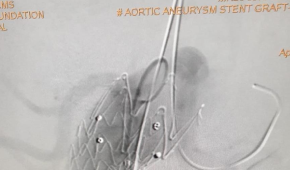
Planned for Left sided Geniculate Artery Embolization in view of recurrent hemarthrosis and left joint pain.
Details about the Procedure/Surgery:
Procedure under local anesthesia. Groin prepared.
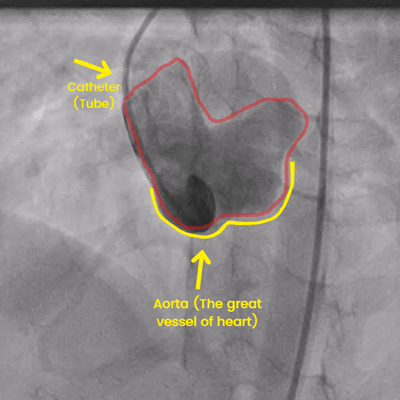
Left Common Femoral Artery antegrade access.
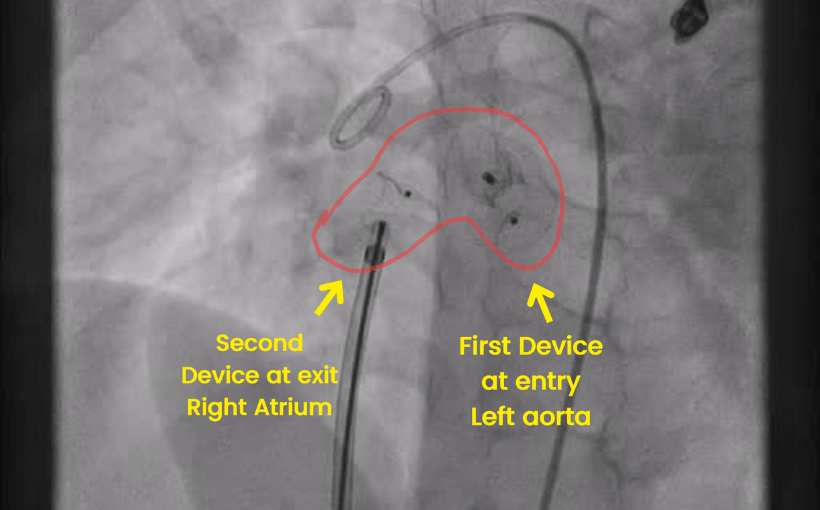
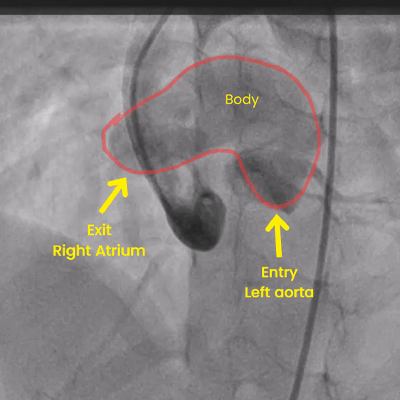
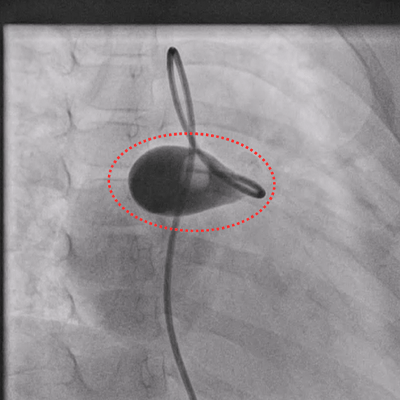
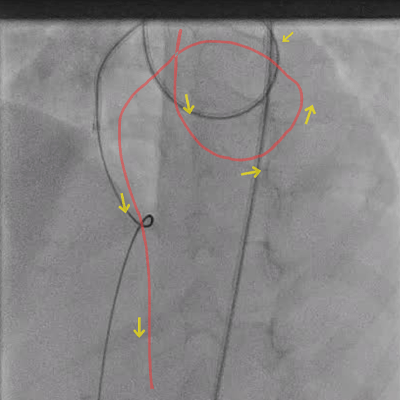
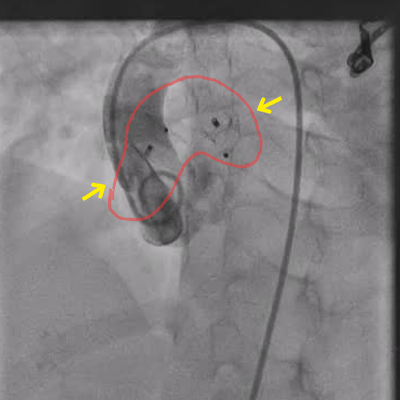
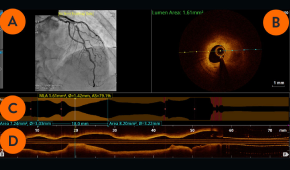
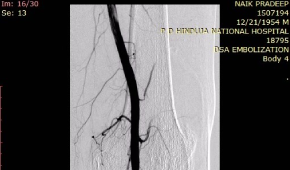
DSA Angiogram done which showed hypertrophied superior and inferior medial geniculate arteries.
Synovial vascular blush noted.
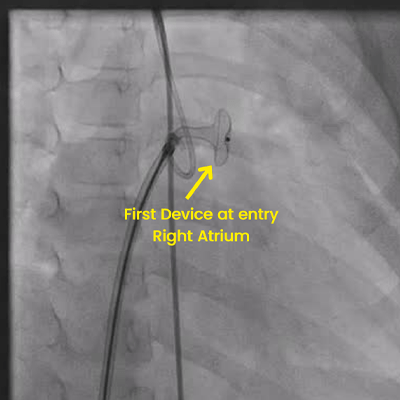
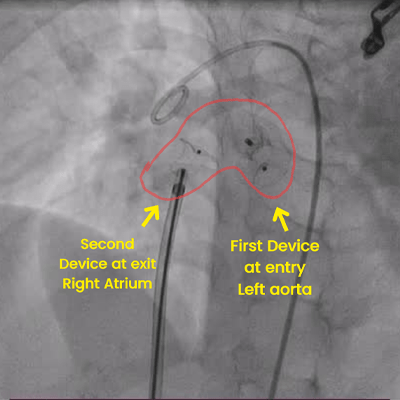
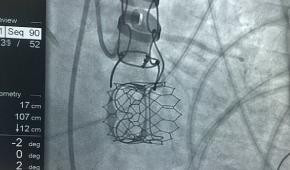
Super selective cannulation of the superior and inferior geniculate arteries done using Progreat microcatheter.
Embolization done with PVA particles.
Post Procedure Details:
Post procedure DSA showed reduction in the synovial vascularity. Reduced arterial blush noted.
Sheath removed by manual compression.
Patient discharged on same day.
Significant reduction of pain on 1 and 3 month follow up.
Conclusion
Geniculate artery embolization (GAE) reduces pain of osteoarthritis by decreasing the vascular supply to the hypertrophied and inflamed synovium and has a role in cases of recurrent hemarthrosis.
It is safe, effective and minimally invasive.
No cuts, no stitches are required.
It can be Performed under local anesthesia.
No general anaesthesia needed.
It is a day care procedure with a same day discharge.